From enabling healthcare providers to deliver patient-centric services to shortening drug discovery lifecycle for pharmaceutical firms, artificial intelligence and its other aspects are revolutionizing our approach toward global healthcare, disease, cure, and prevention. The entire lifecycle of different clinical development processes generates huge amounts of data.
Through strategic applications of different AI tools powered by responsible medical data annotation and abnormality detection, healthcare researchers and physicians are harnessing the potential of this generated data. However, when compared to other fields, there is an inherent ethical imperative that comes with healthcare and is no less than a challenge: ensuring AI systems are free from bias.
Table of Contents
The Rising Demand for Medical Data Annotation
Understanding Different Types of Data Annotation in Healthcare
Bad Bias as a Big Hurdle for AI in Healthcare
The Real-World Impact of Biased Medical AI
Adopting A Multi-Prong Approach to Mitigate Medical Data Biases
The Rising Demand for Medical Data Annotation
Remember when the deadly pandemic COVID-19 brought the entire world to its knees? It served as a wakeup call for the healthcare sector. AI solutions, powered by ethical healthcare data annotation, provide the required accuracy, efficiency, and speed to identify such deadly diseases in advance and take proactive measures. In short, healthcare AI solutions empower providers and patients to take a proactive approach.
“AI will revolutionize the way we live, including our healthcare system.”
Michelle Donelan, Former U.K. Secretary of State for Science, Innovation and Technology
This is evident from the fact that the healthcare data annotation tools market is projected to reach USD 719.15 million by 2030, growing at a CAGR of 27.5%. Such explosive growth highlights the need for accurate annotation across healthcare applications. At the core of these revolutionary tools lies accurately annotated medical data. So, let’s explore the different types of data annotation.
Understanding Different Types of Data Annotation in Healthcare
Medical data is available in different formats: images in the form of X-Rays, CT-Scans, and MRIs, text data in the form of doctor’s notes and prescriptions, and video data in the form of ultrasound, echocardiography, endoscopy, etc. And annotation involves several specialized areas, each requiring unique expertise and ethical considerations. Take a detailed look at these below:
I. Medical Image Annotation
AI can efficiently perform medical image diagnosis and is helping healthcare providers offer reliable and accurate results quickly. This is lifesaving in instances like cancer and tumors, where delayed diagnosis can be fatal. Thus, medical image annotation involves labeling medical images, such as X-rays, MRIs, CT scans, and pathology slides. Annotators identify anatomical structures, abnormalities, and disease markers. And that’s how AI systems are trained for diagnostic imaging, radiology, surgical planning, and more.
II. Medical Text Annotation
From handwritten notes to insurance reports, a lot of medical data is present in the form of text. Medical text annotation, therefore, focuses on clinical notes, research papers, patient records, and pharmaceutical documents. It involves extracting entities, such as symptoms, medications, procedures, and outcomes. This enables natural language processing applications in healthcare documentation and summarization, clinical decision support, and more.
III. Medical Video Annotation
Video annotation is making strides in the healthcare industry by simplifying surgical procedure analysis and strengthening patient monitoring. The healthcare industry uses medical video annotation to label surgical procedures, training videos, and patient monitoring footage. Annotators track instruments, identify surgical steps, and mark critical events. This supports AI development for surgical robotics and promotes improved training for medical professionals.
However, all these types of medical annotation processes and initiatives are considered successful if the models are bias-free. This is possible only when the underlying data annotations are accurate, reliable, and free from bad biases. Otherwise, the consequences will be worse.
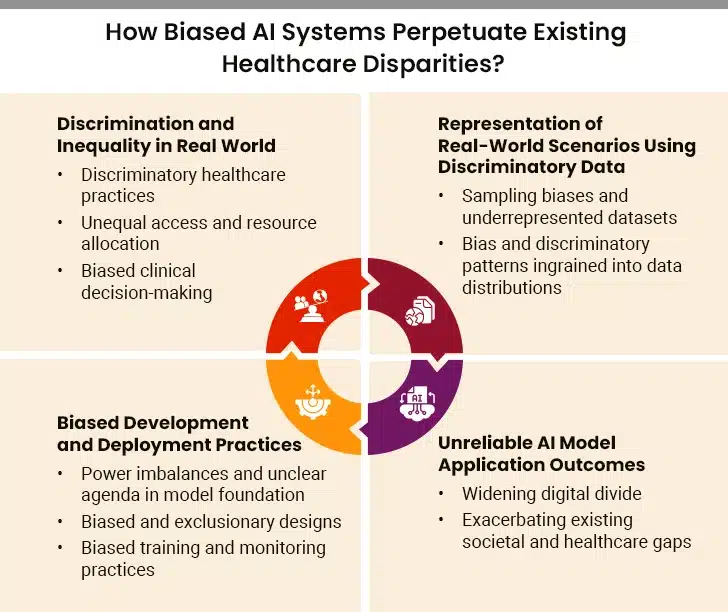
Bad Bias as a Big Hurdle for AI in Healthcare
The root cause of biases in the clinical data is historical health disparities and inequalities in accessing healthcare facilities. For example, when datasets overrepresent a specific demographic, any AI model trained on that dataset will give false or highly inaccurate outcomes for the unrepresented populace. Recent research reveals alarming statistics: medical testing rates for white patients are up to 4.5% higher than for black patients with the same age, sex, medical complaints, and emergency department triage score.
Though seemingly minor on paper, these biases often have serious clinical repercussions. They lead to inaccurate treatment recommendations and misdiagnosis for specific groups. Another issue is the bias creeping within the datasets during data collection. Most data annotation companies collect and process clinical data from different healthcare institutions and hospitals, which cater to a particular population of patients. This leads to unintentional exclusion of other populations.
Additionally, several medical conditions remain underdiagnosed in the marginalized communities, resulting in skewed, inaccurate, incomplete clinical data. Thus, it is vital to understand and navigate these biases to ensure the developed AI-powered tools and systems are accurate and ethical to extend equal care to each patient.
“If there are subgroups of patients who are systematically undertested, then you are baking this bias into your model.”
– Jenna Wiens, Co-Director, AI & Digital Health Innovation
The Real-World Impact of Biased Medical AI
The consequences of biased medical AI extend far beyond statistical errors. A groundbreaking study demonstrates the potential for positive change: correcting racial bias in healthcare could increase the percentage of Black patients receiving additional care from 17.7% to 46.5%. This statistic highlights the current problem’s severity and the tremendous opportunity for improvement through ethical medical data annotation practices.
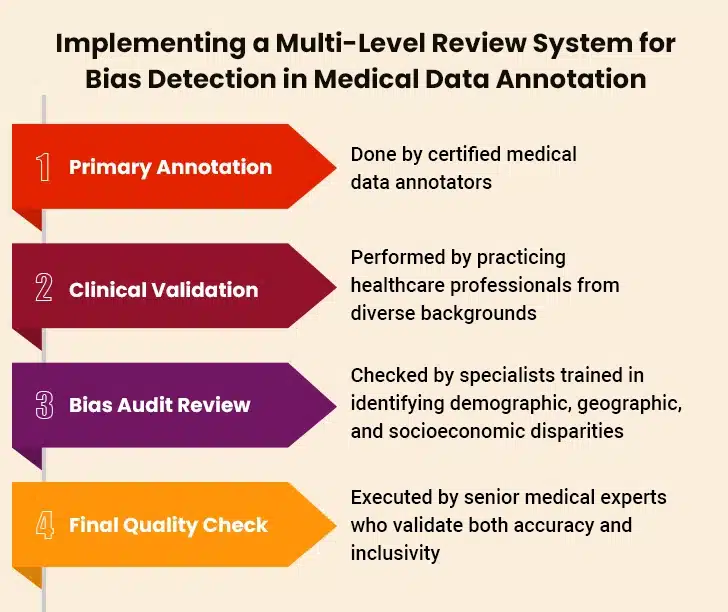
Adopting A Multi-Prong Approach to Mitigate Medical Data Biases
In times when there’s an overload of unstructured data, outsourcing medical data annotation is the right move. But the work isn’t over yet as ethical considerations and data security measures are two areas that require consideration. For healthcare and clinical data, annotators must adopt a multi-faceted approach to mitigate any biases in the four key areas: pharmacovigilance, social listening, patient data security, and medical diagnostics. This must be done while following the industry compliance guidelines and maintaining data confidentiality.
1. Collection & Utilization of Diversified Datasets
For any AI-powered healthcare system or tool to succeed in mass deployment, it is crucial for the training datasets to be sourced from a diverse array of sources.
- Patient Safety and Pharmacovigilance: Datasets developed from varied sources help pharma safety teams monitor and act proactively for any adverse drug side effects across a diversified population. This ensures regulatory compliance during medication safety reporting.
- Social Monitoring: Collecting data from a wide range of patient demographics enables a more holistic monitoring of patient concerns, sentiment, and feedback across different populations.
- Patient Data Protection: Insightful and diverse data helps identify patient data breaches and similar challenges during the development phase of medical devices.
- Improved Diagnostics: Utilizing datasets secured from several demographics helps design more inclusive and accurate diagnostic tools. This significantly reduces the chances of misdiagnosis in an underrepresented population.
2. Employing Transparent Data Collection Measures
Data collection is the first step in the healthcare data annotation process. Ensure complete transparency in the data collection process with clear documentation of the source of data and collection methodologies.
- Patient Safety and Pharmacovigilance: Maintaining transparency in data collection processes enhances traceability and accountability in pharmacovigilance initiatives. This optimizes the capability to immediately detect and document negative outcomes.
- Patient Data Protection: Transparency in data collection processes helps secure intellectual property by offering clear, detailed documentation on sources of data and methodologies adopted to collect that information.
- Improved Diagnostics: Following transparent data collection processes is vital to validate the accuracy and fairness of various diagnostic tools while obtaining regulatory approvals.
3. Regular Algorithmic Audits
Frequent and detailed audits of datasets by annotation companies are a must for detecting and rectifying biases. This also ensures that the outcomes are accurate and reliable.
- Pharmacovigilance and Patient Safety: Regular and thorough audits help detect trends and patterns in harmful events, especially when analyzing a diverse range of patient demographics.
- Social Listening/Monitoring: Regular algorithms and processes audits for social listening ensure efficient data collection and analysis from different data sources and populaces.
- Patents/IP Protection: End-to-end audits examine datasets for trends that pinpoint the improper utilization of confidential data, further assisting in detecting IP infringements.
- Diagnostics: Auditing datasets sourced from diagnostic tools regularly helps maintain their capability to generate unbiased and consistent results for patients from diverse demographics, thus improving overall diagnostic accuracy.
4. Regulatory Compliance
It is paramount for AI tools in healthcare to adhere to industry guidelines and regulatory standards to ensure that all ethical considerations are addressed systematically.
- Pharmacovigilance and Patient Safety: Strict adherence to regulatory policies and industry standards during data annotation in pharmacovigilance is vital. This ensures complete reporting compliance and patient safety.
- Social Listening/Monitoring: Enforcing regulatory compliances during social listening strategies ensures patient privacy by strictly adhering to data security and privacy.
- Patents/IP Protection: Following clear IP regulations while processing and annotating data helps protect patent and IP rights. This is especially important in an industry like health sciences, where research, patents, and intellectual property rights play a critical role.
- Diagnostics: Following regulations optimizes the opportunity for safe and effective utilization of AI diagnostic tools in clinical environments. Moreover, this is essential for securing regulatory endorsement.
5. Continuous Training
Data annotators and AI model developers must be trained about ethical considerations and the latent repercussions of bias in clinical data. This is essential to foster the culture of responsible AI utilization in healthcare and medical sciences.
- Pharmacovigilance and Patient Safety: Regular training on measures to implement safety regulations while collecting data and understanding their importance is vital in pharmacovigilance.
- Social Listening/Monitoring: Providing ethical AI and data collection training ensures that data experts engaged in social listening are well-aware of the potential consequences of bias in data collection, processing, and annotation.
- Patents/IP Protection: Holistic training on protection of intellectual property rights is very important for data annotators. It helps them navigate through the complicated patent route in medical sciences and healthcare.
- Diagnostics: Regular training reinforces the importance of meeting ethical standards while developing AI-powered diagnostic tools to mitigate any kind of biasness in the results.
How Outsourcing Data Annotation Services Can Supercharge Your AI Model?
Wrapping Up
Recognizing, understanding, and addressing various biases within AI-driven healthcare systems and tools is vital to ensure equitable and accurate health outcomes for all populaces. As part of an industry-wide initiative, the need of the hour is to prioritize the development of highly transparent, fair, and inclusive AI systems.
Enhancing real-world medical data quality becomes streamlined when organizations outsource data annotation in healthcare to professionals who are thorough, efficient, and precise. Moreover, the future of healthcare depends on our collective commitment to ethical AI development. And it starts with the fundamental building blocks of well-annotated, diverse, and representative training medical data.
Thus, all the verticals and domains in the healthcare sector looking to harness the potential of AI, the first step is to invest in high-quality, accurate, and bias-free medical data annotation services.