What if your doctor had assistants that could spot hidden patterns in scans or predict a health risk with uncanny accuracy? This is no longer hypothetical. Artificial intelligence (AI) has become that indispensable partner today.
Most healthcare organizations now use AI. It is changing how medical professionals diagnose illnesses and treat patients. The field is experiencing rapid expansion.
Modern healthcare providers are seeing worthwhile returns on their AI investments. Hospitals and clinics often achieve measurable benefits relatively quickly after implementing AI. While financial gain is a clear outcome, it isn’t the only driver for adopting this technology.
AI tools help medical professionals work smarter, not harder. AI applied to medical imaging helps detect serious conditions earlier than many conventional approaches. AI also helps manage hospital operations more effectively.
The key insight? AI reinforces human expertise instead of replacing it. Medical professionals still make important decisions. However, they now have powerful tools that can analyze vast amounts of data to identify disease markers that might otherwise go unnoticed. This partnership between human judgment and machine learning analysis has led to personalized treatments and better patient outcomes.
Table of Contents
Key Applications of AI Enhancing Medical Expertise
AI keeps making its way into healthcare, and some applications stand out because they help boost medical expertise. These technologies do not replace human judgment. They give doctors and nurses better tools to do things that were not possible before.
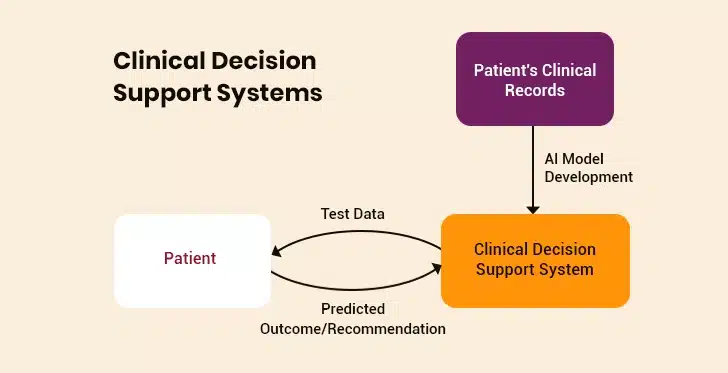
1. Clinical Decision Support Systems
Medical professionals now use AI as an intelligent assistant in daily practice. Nearly two-thirds of physicians (66%) are now using AI in healthcare. Among these adopters, 21% use AI for documentation of medical charts and billing codes, while 20% employ it for creating discharge instructions and progress notes.
The impact on clinical decision-making shows tremendous promise. Physicians who receive AI assistance make more accurate medical choices. In tasks involving complex treatment decisions, AI significantly improves physician performance.
However, better care doesn’t mean unfair treatment. Research shows that AI tools help doctors make more accurate decisions without introducing new biases or worsening existing ones. Because of this success, a majority of doctors believe AI tools will be crucial in future clinical decision-making.
2. Diagnostic Excellence Through AI
AI shines when it comes to pattern recognition and anomaly detection. Take radiology, where hospitals perform billions of imaging procedures annually. Here’s a staggering fact: approximately 97% of this imaging data traditionally went unused. Today, machine learning helps healthcare professionals structure, index, and use this information for more accurate diagnostics.
Modern AI systems detect ailments like pneumonia from radiographs much more accurately than human radiologists. AI particularly excels at the early detection of breast cancer. Using AI systems for interpreting mammograms reduces the incidence of false positives and false negatives. When examining skin cancer, deep learning models diagnose melanoma cases with remarkable accuracy and even recommend treatment options.
3. Patient Monitoring and Preventive Care
AI in the healthcare industry helps with continuous monitoring and prevention. AI-enabled tools allow nurses and care teams to spot early signs of serious conditions. This enables rapid response. Advanced AI systems monitor vital signs and calculate risk scores automatically. This helps hospitals reduce serious adverse events such as cardiac arrest.
Stroke care benefits from AI that examines CT images to detect large vessel occlusion and its location. This analysis is then shared with physicians and intervention centers. For cardiac care, AI helps with the timely detection of atrial fibrillation (irregular heartbeat) by studying electrocardiogram recordings.
4. Operational Efficiency and Administrative Support
Physicians see administrative burden reduction as the most promising use of AI, with a majority citing it as the biggest opportunity area. AI simplifies workflows by automating documentation, optimizing scheduling, and managing patient flow.
AI-based tools assist with documentation and content summarization. This helps clinicians maintain accurate medical records. AI systems also allow seamless exchange of information between different hospital departments. This speeds up many back-office tasks, including billing.
AI-based healthcare assistants can answer questions related to medication and the availability of doctors. They also help patients book appointments with their physicians. This reduces the workload of clinical staff. It also allows them to focus on treating patients with empathy and care.
As healthcare keeps changing, the best AI systems will be those that support collaborative partnerships between technology and human expertise. The goal stays consistent: give medical professionals better tools to extend their skills, reduce burnout, and improve patient outcomes.
AI Agents: 7 Game-Changing Use Cases Transforming Modern Businesses
Real-World Implementation: Case Studies from Leading Healthcare Institutions
Today, hospitals and clinics are moving beyond pilot programs. These organizations have deployed AI systems that deliver measurable results, providing clear roadmaps for others looking to follow suit.
I. Mayo Clinic
Mayo Clinic uses AI to turn complex medical data into practical insights for doctors. A key focus is predicting kidney failure in patients with polycystic kidney disease. Their AI analyzes patient scans to measure kidney size, applies a special Mayo classification system, and forecasts how the disease might progress. This allows doctors to plan early treatments like dialysis or transplants.
Mayo also uses AI-based tools to help doctors manage sudden kidney injuries. These systems predict risks and spot problems early. They also suggest personalized treatments, such as adjusted medication doses.
Crucially, Mayo’s “AI Factory” platform, developed with Google, lets clinicians build their own AI tools safely. This approach encourages innovation from medical teams using this technology.
II. Google DeepMind
Google DeepMind focuses on major biomedical breakthroughs and making AI tools accessible. Its AlphaFold system predicts the complex 3D shapes of millions of proteins and how they interact with human cells. This speeds up research for new drugs.
DeepMind’s commercial spin-off, Isomorphic Labs, uses this AI foundation to design new medications. They aim to bring these AI-created drugs into human testing soon, potentially changing how drugs are discovered.
To help hospitals directly, DeepMind has recently released MedGemma. This open-source AI model is designed for medical tasks. Developers can use it to build tools, such as systems that help analyze X-rays or summarize patient notes. These solutions will make it easier for hospitals to adopt AI.
III. Community Hospitals
Academic medical centers often lead AI adoption, but community hospitals are proving that big budgets aren’t required. Flagler Hospital in Florida has implemented an AI system for building pneumonia care pathways. The pathways reduce patients’ length of stay and lower their readmission rates.
These case studies share common success factors. They focus on fixing specific clinical or operational problems instead of using technology without purpose. Clear success metrics come before deployment. Clinical staff participate throughout development to ensure AI tools fit smoothly into their existing workflows.
examples prove the value of AI in healthcare comes from improving human expertise. AI provides tools that extend what clinicians can do. It also lets them focus on the human aspects of care that machines can’t imitate.
Challenges and Limitations: What Stands in the Way
AI implementation in healthcare is no easy undertaking. Real-world deployment faces obstacles that can affect even the most promising projects. Leading healthcare organizations address these challenges head-on.
1. Data Privacy and Security
Implementing AI in healthcare management needs lots of data, which raises serious privacy concerns. Research shows that truly anonymous health data is unattainable. Many times, algorithms can reidentify individuals even when their protected health information has been stripped out. The risk grows bigger when this sensitive medical data moves to public cloud servers for processing. This creates lasting consequences: workplace discrimination and inflated insurance premiums.
Regulatory compliance complicates matters further. The European Union’s GDPR says patients own their data and must agree before anyone uses or shares it. However, healthcare leaders argue that existing laws haven’t kept pace with new technology. This creates uncertainty around the accountability of AI systems.
2. Bias and Fairness Issues
AI systems can amplify existing inequities across socioeconomic status, race, ethnicity, gender, and other factors. Bias may come in at multiple stages:
- Data Preparation: Most datasets overrepresent Caucasian patients
- Model Development: Algorithms learn from historically biased treatment decisions
- Evaluation: Overreliance on certain metrics obscures biased performance
- Deployment: End-user interactions introduce additional bias
The consequences can be severe. To cite an example, a healthcare AI algorithm may prioritize patients from a particular community because it was trained on biased datasets. The issue can be mitigated through many methods—pre-processing data through sampling, mathematical approaches during model training, and post-processing techniques. However, no method can eliminate bias completely.
3. The Black Box Problem
Complex AI models often work like black boxes. As a result, doctors can’t see how these models reach conclusions. This lack of explainability creates practical problems. Clinicians can’t effectively:
- Assess if the parameters used make clinical sense
- Identify when a system might be making errors due to bias
- Explain decisions to patients, potentially damaging the doctor-patient relationship
- Contest or modify wrong decisions
Building explainable artificial intelligence for healthcare requires balancing detail with usability. Overly technical information may overwhelm clinicians. Highly simplified explanations might leave out critical details. The solution lies in providing context-specific explanations that help clinicians understand why the AI reached its conclusion.
4. Adoption Barriers in Practice
Even the most advanced AI technology can fail if adoption barriers get in the way. Healthcare providers face many such challenges:
- Staff concerns represent significant obstacles to AI adoption, including training gaps.
- Physicians may resist AI because they don’t understand it, worry about losing their jobs, or fear changes to their work.
- Limited training in evaluating AI software makes it difficult for clinicians to assess system reliability.
Financial constraints also impede adoption. Organizations need to spend money on keeping AI running, getting expert assistance with training data, and building better infrastructure. The Harris Poll survey has found that while 97% of healthcare organizations see AI as vital in the next 5 years, only 54% of IT leaders feel confident to make it work.
Organizations can solve these challenges through focused approaches. They should engage with healthcare specialists who champion AI, focus on tools with clear efficiency gains, and create transparent governance structures to address concerns systematically.
Generative AI in Healthcare: The Future of Patient Care and Medical Advancements
Integrating AI into Clinical Workflows: Prerequisites for Success
Healthcare organizations need strategic planning when they integrate artificial intelligence and healthcare. Their medical facilities should meet specific requirements so AI can improve clinical workflows without causing disruption.
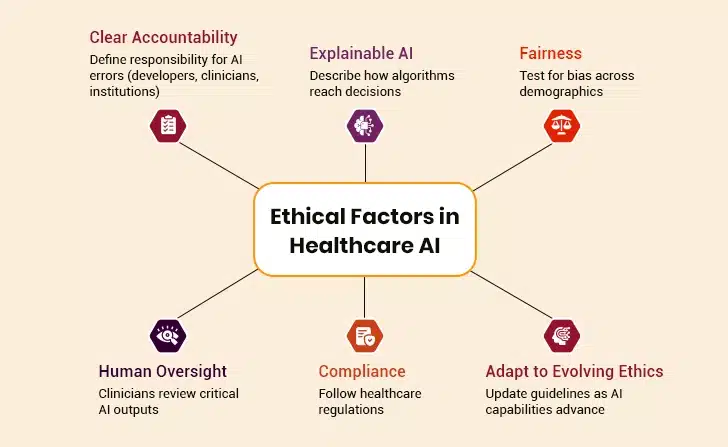
I. Emphasize Human-in-the-Loop Models
Healthcare organizations must keep the “human-in-the-loop” approach at their core for responsible AI deployment. This model allows clinicians to keep their decision-making authority while AI provides additional insights. Physicians need to review AI suggestions before putting them into action. These suggestions could range from patient email responses to medical record documentation and risk predictions.
A well-laid-out human-in-the-loop framework brings together different stakeholders in governance structures. These include developers, patients, clinical staff, IT personnel, and ethics specialists. Healthcare organizations can tackle critical AI system concerns throughout their lifecycle with this approach.
II. Focus on Clear Returns
Healthcare organizations get the best results when they implement AI solutions that deliver measurable gains. These solutions bring results by reducing operational costs, easing staff burden, and allowing more attention to patient care. To cite an example, AI that automates clinical notes can save the time doctors spend on paperwork. This helps them see more patients.
AI systems that predict which patients might require readmission help hospitals use resources more efficiently. Automating complicated insurance approvals with AI speeds up the process. Starting with these practical areas creates quick wins. It also builds momentum for the wider adoption of AI.
III. Establish Oversight and Audit Systems
Healthcare organizations must set up structured audit processes as regulatory frameworks change. Medical algorithmic audits help evaluators spot potential errors and prepare for potential risks. These audits should check AI systems’ functionality, transparency, ethical behavior, and compliance.
Organizations should create dedicated committees with experts from various fields to oversee AI deployment. They should also ensure safety protocols are followed. These committees must review new AI applications regularly. In addition, they should develop processes to track their performance.
A detailed emergency protocol is also crucial. Organizations need procedures to shut down AI systems if something goes wrong. This approach makes sure that AI integration improves rather than compromises patient care.
Wrapping Up
Artificial intelligence works best as a partner to medical expertise, not a replacement. Organizations that understand this partnership see measurable benefits. These include improved diagnostic accuracy, streamlined processes, and reduced administrative work.
Yet its implementation involves challenges. These include data privacy concerns, algorithmic bias, and adoption barriers. Healthcare organizations can solve these issues with robust governance frameworks, diverse training data, and transparent models.
Healthcare AI is neither a cure-all nor a threat to medical professionals. It provides tools that can solve major healthcare challenges when properly implemented. The organizations that succeed will be those that see both the promise and the limits of these technologies while maintaining dedication to patient well-being.
After all, the true measure of the success of AI and healthcare remains improved patient outcomes through augmented, not replaced, medical expertise.